Poor
CD4 Cell Recovery on Antiretroviral Therapy Is Linked to Late Treatment,
Leads to Adverse Outcomes
 |
 |
 |
 |
 |
 |
 |
| SUMMARY:
People with HIV who do
not experience significant CD4 cell recovery with antiretroviral
therapy (ART) -- even though they achieve viral load suppression
-- are at risk for a host of complications including cardiovascular
disease and cancer, according to an analysis of the Dutch
ATHENA cohort presentation at the 17th
Conference on Retroviruses and Opportunistic Infections (CROI
2010) last week in San Francisco. In related news, researchers
with the DART trial in Africa found that starting treatment
late increased the likelihood of inadequate CD4 cell gains.
|
|
 |
 |
 |
 |
 |
 |
 |
By
Liz Highleyman
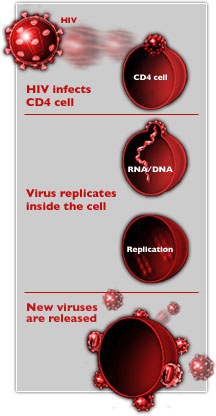 Despite
achieving full suppression of plasma HIV RNA, an estimated 5% to 10%
of patients have incomplete immune recovery, a phenomenon know as discordant
response.
Despite
achieving full suppression of plasma HIV RNA, an estimated 5% to 10%
of patients have incomplete immune recovery, a phenomenon know as discordant
response.
ATHENA
Steven van Lelyveld and colleagues looked at the relationship between
incomplete immune recovery and the occurrence of cardiovascular
events, cancer, and other adverse outcomes, which they hypothesized
might be due to ongoing immune deficiency.
The analysis included 3071 participants in ATHENA, a national observational
study of people with HIV/AIDS in the Netherlands. Selected patients
had started ART since 1998, achieved virological suppression (< 500
copies/mL) within 9 months of treatment initiation, maintained suppression
for at least 2 years, and had undetectable viral load during the prior
6 months. Pregnant women and people taking immunosuppressive drugs were
excluded.
Most participants (about 80%) were men, the mean age was 41 years, and
sex between men was the most frequent HIV risk factor. The median CD4
cell count at baseline was fairly high, at 425 cells/mm3, but the nadir
(lowest-ever) level was 160 cells/mm3. Nearly 60% were taking non-nucleoside
reverse transcriptase inhibitors (NNRTIs)
and about one-third were on protease
inhibitors. As in many European cohorts, smoking was common (about
60%).
Participants were allocated to 4 groups according to immune recovery,
as indicated by CD4 cell counts after 2 years on treatment: < 200
(6.6%), 200-350 (21.0%), 350-500 (46.0%), and > 500 (26.4%) cells/mm3.
For comparison, the normal range for healthy HIV negative adults is
around 500-1500 cells/mm3.
Results
 |
A
total of 2048 patients experienced CD4 cell gains of at least 100
cells/mm3. |
 |
Patients
with incomplete immune recovery after 2 years were significantly
older than those with larger CD4 cell gains. |
 |
198
total endpoint events occurred during follow-up, including new cardiovascular
events, new malignancies, AIDS-defining events, and death. |
 |
Combined
endpoint events were significantly more likely to occur in people
with < 200 cells/mm3. |
 |
58
participants developed cardiovascular disease during follow-up. |
 |
Here
too, people with a baseline CD4 count < 200 cells/mm3 had a significantly
elevated risk. |
 |
36
participants developed non-AIDS malignancies. |
 |
There
was a trend toward a link between being in the lowest CD4 cell category
and shorter time to non-AIDS malignancies, but this did not reach
statistical significance. |
 |
After
taking into account confounding factors including sex and age, adjusted
hazard ratios relative to the < 200 cells/mm3 group for the combined
endpoints were: |
| |
 |
0.67
for people with 200-350 cells/mm3; |
 |
0.57
for those with 350-500 cells/mm3; |
 |
0.46
for those with > 500 cells/mm3. |
|
 |
Incomplete
immune recovery after 2 years on suppressive ART was significantly
associated with older age, male sex, lower nadir CD4 count, lower
HIV RNA at ART initiation, and starting with a NNRTI rather than
a protease inhibitor. |
DART
The second
study looked at the link between poor CD4 cell recovery and adverse
outcomes in a resource-limited setting.
The DART trial enrolled 3316 previously untreated HIV positive adults
in Uganda and Zimbabwe with a low median CD4 count of 86 cells/mm3.
Participants started 1 of 3 ART regimens, using zidovudine/lamivudine
(Combivir) plus either tenofovir
(Viread)(74%), nevirapine
(Viramune)(16%), or abacavir
(Ziagen)(9%). Participants were randomly assigned to be followed
using either laboratory and clinical monitoring or only clinically-driven
monitoring, switching to second-line ART when they either fell below
100 cells/mm3 or develop WHO stage 4 disease.
Results
 |
After
a median 5 years of follow-up, 69% of patients ever achieved a confirmed
CD4 count >250 cells/mm3 on their first-line regimen,
46% reached 350 cells/mm3, and 19% reached >500 cells/mm3. |
 |
Patients
on first-line therapy took a median 1.8 years to reach >250
cells/mm3, 3.9 years to reach 350 cells/mm3, and more than 6 years
to reach >500 cells/mm3. |
 |
Among
participants who stayed on their first-line regimen for 1 year before
switching: |
| |
 |
10%
still had a CD4 count <99 cells/mm3 or less; |
 |
38%
had 100-199 cells/mm3; |
 |
39%
had 200-349 cells/mm3; |
 |
10%
had 350-499 cells/mm3; |
 |
2%
had 500 cells/mm3. |
|
 |
By
5 years after ART initiation, the proportion reaching >500
cells/mm3 had increased, but still remained relatively low at 21%.
|
 |
20%
of patients with a CD4 count < 100 cells/mm3 after 1 year, and
55% with 100-199 cells/mm3, subsequently reached >250,
the level at which AIDS-related opportunistic infections become
very uncommon. |
 |
However,
the rate of CD4 count change from week 24 to 48 did not predict
who would or would not eventually reach >250. |
"Patients
initiating ART with very low CD4 counts struggle to achieve sufficient
immune restoration within 2 to 3 years though responses continue to
improve over time," the researchers concluded.
They added
that people with a CD4 count < 125 cells/mm3 after week 48 on ART
are not likely to ever reach >250 cells/mm3 on the first-line
regimen.
The investigators
stated that these findings "highlight the importance of expanded
earlier diagnosis and treatment initiation" in resource limited
settings. They also raised the prospect of switching people with limited
CD4 cell recovery -- even if they have suppressed viral load -- to second-line
regimens associated with larger CD4 cell gains, including protease inhibitors
rather than NNRTIs, and potentially maraviroc
(Selzentry).
Study
1: University Medical Center Utrecht, Netherlands; Stichting HIV Monitoring,
Amsterdam, Netherlands.
Study
2: Medical Research Council/Uganda Virus Research Institute, Entebbe,
Uganda; Medical Research Council Clinical Trials Unit, London, UK; Joint
Clinical Research Center, Kampala, Uganda; University of Zimbabwe, Harare,
Zimbabwe; Infectious Diseases Inst, Makerere University, Mulago, Uganda;
Imperial College London, UK.
2/23/10
References
S van
Lelyveld, L Gras, A Kesselring, and others. Incomplete Immune Recovery
on HAART Is Associated with Significant More Cardiovascular Events and
a Trend Towards More Non-AIDS Related Malignancies in Dutch ATHENA Cohort.
17th Conference on Retroviruses & Opportunistic Infections (CROI
2010). San Francisco. February 16-19, 2010. (Abstract
714).
P Munderi,
AS Walker, C Kityo, and others. Immune Restoration over 5 Years on ART
among Patients Initiating Treatment with Advanced Immune Deficiency
in the DART Trial in Uganda and Zimbabwe. 17th Conference on Retroviruses
& Opportunistic Infections (CROI 2010). San Francisco. February
16-19, 2010. Abstract 110.