Endothelial
Dysfunction Is Worse in People with HIV/HCV Coinfection, but Improves
with Sustained Response to Hepatitis C Treatment
 |
 |
 |
 |
 |
 |
 |
| SUMMARY:
HIV/HCV coinfected people have higher levels of 2 biomarkers
of endothelial (blood vessel) dysfunction compared to individuals
with neither virus, researchers reported in a poster presentation
at the 17th Conference on Retroviruses
and Opportunistic Infections (CROI 2010) last week in
San Francisco. Levels of sICAM-1 and sVCAM-1 decreased significantly,
however, among patients who received interferon-based hepatitis
C treatment and achieved a sustained virological response
(SVR), suggesting that this may decrease their risk of cardiovascular
disease. |
|
 |
 |
 |
 |
 |
 |
 |
By
Liz Highleyman
Chronic
hepatitis C virus (HCV) infection can progress to advanced liver
disease, including cirrhosis
and hepatocellular
carcinoma, and this may happen more rapidly in HIV/HCV
coinfected individuals. But people with chronic HIV and/or HCV infection
are also at higher risk for a host of other conditions not directly
caused by these viruses.
Prior
studies in both HIV negative and HIV/HCV coinfected populations have
shown that people treated with interferon-based
therapy have reduced odds of liver disease progression and liver-related
death, especially if they achieve SVR, or a "cure."
 At
CROI, Juan Berenguer presented data showing
that sustained response to hepatitis C treatment not only reduces rates
of liver-related complications and death in coinfected people, but also
decreases the risk of AIDS-defining conditions, AIDS-related death,
and death due to other causes.
At
CROI, Juan Berenguer presented data showing
that sustained response to hepatitis C treatment not only reduces rates
of liver-related complications and death in coinfected people, but also
decreases the risk of AIDS-defining conditions, AIDS-related death,
and death due to other causes.
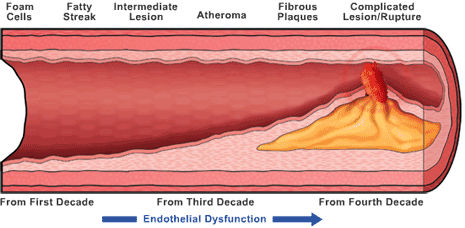
Cardiovascular
disease has become an increasingly important cause of death as people
with HIV live longer. A growing body of evidence suggests that chronic
viral infection can trigger ongoing immune activation and inflammation
that causes problems throughout the body. Among these is atherosclerosis,
or "hardening of the arteries," which can lead to blockage
of blood vessels causing a heart attack or stroke.
In their
CROI poster, Isabel Fernandez de Castro from Istituto de Salud Carlos
III in Madrid and colleagues assessed whether endothelial (blood vessel
lining) dysfunction in HIV/HCV coinfected individuals is a consequence
of HIV infection, HCV infection, or both.

To do
this, they measured 2 blood biomarkers of endothelial injury, soluble
intercellular adhesion molecule (sICAM) and soluble vascular cell adhesion
molecule (sVCAM). Both substances have been linked to atherosclerosis
and increased risk of cardiovascular events.
This cross-sectional study included 183 HIV/HCV coinfected patients
taking combination antiretroviral therapy (ART) and 24 healthy control
participants not infected with either virus. Most (75%) were men, the
average age was 39 years, and 90% had a history of injection drug use.
With regard to baseline HIV status, participants had been on ART for
a median duration of about 4 years, a majority had HIV RNA < 50 copies/mL,
the median current CD4 cell count was 476 cells/mm3, and the median
CD4 cell nadir (lowest-ever level) was 196 cells/mm3. Looking at hepatitis
C status, the estimated duration of HCV infection was 21 years, about
60% had hard-to-treat HCV genotype 1, nearly one-quarter had high HCV
viral load, and about one-third had advanced liver fibrosis or cirrhosis
(stage F3-F4).
A total of 32 coinfected patients (17.4%) were treated with interferon-alfa
(pegylated or conventional was not stated) plus ribavirin for 48 weeks.
Results
 |
HIV/HCV
coinfected individuals had significantly higher levels of both sICAM-1
and sVCAM-1 compared with the uninfected control group. |
 |
Patients
with HCV genotype 1, advanced fibrosis (stage F3 or higher), and
moderate-to-severe histological activity (grade A2 or higher) had
the highest sICAM-1 and sVCAM-1 levels. |
 |
In
a univariate (single factor) analysis, elevated sICAM-1 and sVCAM-1
levels were significantly associated with CD4 cell count, time on
ART, insulin resistance, HCV genotype 1, and advanced fibrosis. |
 |
In
a multivariate analysis controlling for other factors, only HCV
genotype 1 and advanced fibrosis remained significant predictors
of elevated sICAM-1. |
 |
These
same 2 factors plus longer time on ART were significantly associated
with elevated sVCAM-1. |
 |
sICAM-1
and sVCAM-1 levels were also positively correlated with elevated
levels of circulating liver enzyme (ALT, AST, and alkaline phosphatase). |
 |
Looking
at hepatitis C treatment response, non-responders had significantly
higher sICAM-1 and sVCAM-1 levels. |
 |
Patients
who achieved SVR had significantly reduced sICAM-1. |
"HIV
and HCV coinfection induces alterations in plasma endothelial adhesion
molecules," the investigators concluded. "Therefore, the cardiovascular
risk is increased in HIV/HCV coinfected patients in an advanced stage
of chronic hepatitis C infection."
Instituto de Salud Carlos III, Madrid, Spain; Hosp Univ Gregorio
Marañon, Madrid, Spain.
2/23/10
Reference
I
Fernández de Castro, J Berenguer, D Micheloud, and others. Hepatitis
C Infection Increases Endothelial Dysfunction in HIV/HCV Co-infected
Patients. 17th Conference on Retroviruses & Opportunistic Infections
(CROI 2010). San Francisco. February 16-19, 2010. Abstract 667.